Reflections of Career Air Force Hand Surgeon
** This is the author’s opinion and does not represent the military or U.S. government. **
By John V. Ingari, MD
When asked to reflect on my hand surgery career in the United States Air Force a flood of thoughts emerged. I spent 25 years on active duty, beginning as a second lieutenant in 1982. I retired from active service in 2007 as a full colonel, now 12 years ago. My memories include being deployed for over 2 and ½ years in war zones, as well as multiple overseas bases, along with my peacetime assignments throughout the United States for the rest of the 25 years. There were too many highlights to list here, but the enduring friendships I made, the collegial practice environment, and the emphasis on teamwork made my time in the Air Force seem far more of a privilege than a duty. As the deputy commander of the largest Air Force Theater Hospital in Iraq in 2005-6, I found performing wartime surgery was professionally the most challenging, rewarding, yet humbling experience of my career.
But it is actually one “peacetime” case that stands out as an embodiment of what I think the military hand surgery experience represents. I am going to relate that story.
April 15th, 2002, “tax day”, now some 16 years ago, I was at Wilford Hall Medical Center at Lackland Air Force Base, as the Chief of Hand Surgery. Wilford Hall served as one of three Levels I trauma centers for San Antonio, with the “County Hospital” (University of Texas Health Sciences Center at San Antonio) and Brooke Army Medical Center (BAMC), serving as the other trauma centers. A call came to our emergency department letting me know that both the County Hospital and BAMC were unavailable to take a patient with a severed hand, and, “Could you take the patient”?
I answered yes, and that began a daylong episode I remember well to this day. The patient arrived to the Emergency Department, along with his completely amputated hand, at the level of the carpus, suffered in a power saw injury. After a ten-minute evaluation of the patient, and the severed hand, with time for a CBC, type and cross, radiographs of the residual limb and hand, we proceeded to the OR. The patient was strangely serene, and simply wanted to know if we could reattach his hand. I had already contacted the other Air Force staff hand surgeon, along with several residents, two of whom are practicing hand surgeons today, to ask for help. That help, along with some help from “above” led to a very memorable experience.
One resident worked on the amputated hand, labeling each tendon with a Kessler suture and a Steri Strip to annotate each flexor and extensor tendon. I began work, with another resident on the residual limb, exposing arteries, nerves, tendons and bone. It was clear that the carpus was not salvageable due to the power saw injury, so I made the decision that a wrist fusion would be optimal for bony fixation.
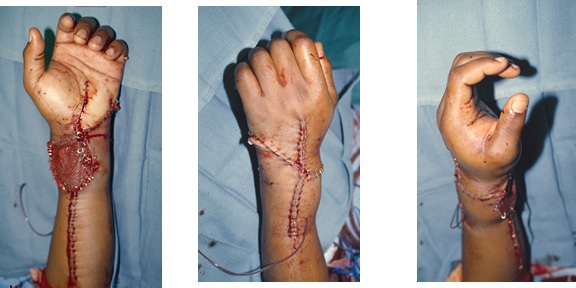
The decision for arterial anastomosis was based on the patient’s anatomy. The radial artery had a considerably larger caliber than the ulnar artery, so the radial artery was chosen for anastomosis. Two large dorsal veins were selected for venous anastomoses. Within four hours of presentation to our Emergency Department, blood flow was reestablished to the severed hand, along with bony fixation and multiple tendon and nerve repairs. We had prepared for a skin graft, and one was definitely needed to allow soft tissue coverage in the swollen wrist. A carpal tunnel release was also done following reattachment.
While the details of the case remain etched in my brain, what I remember most vividly are the people and the circumstances surrounding the case. I have a treasured photograph of one of the residents, proudly showing the hand, with each tendon marked, nerves and vessels ready to go, just prior to reattachment. I remember being told that Wilford Hall was selected only after the County Hospital and BAMC were called. I remember virtually everyone I asked for help, dropping everything from clinic to elective surgeries to assist in the case. I remember thinking, retrospectively, how quickly decisions were made with regard to wrist fusion, which vessels would be best for anastomosis and that we remembered to “prep” the leg, “in case” a skin graft might be needed.
One final thought: The reason we were able to do this case was because my mentors taught me well. Dave Green, Chris Pederson, Eugene (Tom) O’Brien, and Bill Sanders had given me the “tools” needed during hand fellowship that made this case successful. Our teachers make us who we are, and a little help from “above,” during a crisis, is also a good thing.
While this single case cannot encompass the myriad of experiences that make military hand surgery unique, the teamwork, mentorship, forged friendships, and sense of duty to help those in need, were definitely what I remember as making service to one’s country as a military physician a true privilege.


Dr. John V. Ingari
Johns Hopkins Orthopaedics
Comment (1)
fred corley
May 9, 2019 8:53 pmgreat job from a fine surgeon and good friend
thanks for your service
Fred